Body Dysmorphic Disorder (BDD) Symptoms: Causes, and Therapy Options
Contents
Introduction
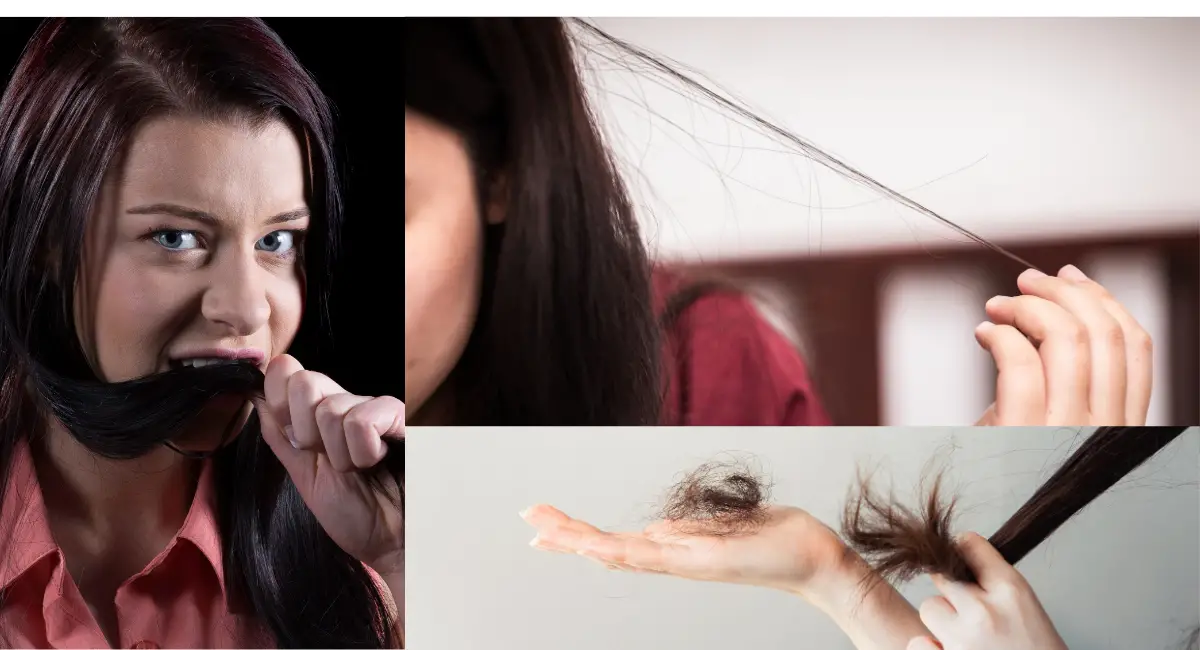
Body Dysmorphic Disorder (BDD) is a mental health disorder characterized by an intense preoccupation with one or more perceived defects or flaws in physical appearance, which are either not observable or appear minor to others. Individuals with BDD often feel ashamed, anxious, or distressed about their appearance and may engage in repetitive behaviors such as excessive grooming, mirror checking, or seeking reassurance. This disorder can significantly impair daily functioning, social interactions, and quality of life.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), BDD affects approximately 1-2% of the population, and its severity can range from mild preoccupation to extreme levels of distress that interfere with normal life. One specific subtype of BDD is Muscle Dysmorphia, where the individual is preoccupied with the belief that their body is insufficiently muscular or lean. This article will explore Body Dysmorphic Disorder, including the subtype of Muscle Dysmorphia, focusing on the Symptoms, Causes, and Therapy Options available..
Common Symptoms of Body Dysmorphic Disorder (BDD)
BDD involves obsessive thoughts about physical appearance and compulsive behaviors aimed at correcting or hiding perceived flaws. Below is a table outlining the common symptoms and examples of how they manifest in daily life:
| Symptom | Description/Example |
|---|---|
| Preoccupation with Appearance | Persistent thoughts about a perceived flaw in physical appearance. For example, someone may believe their skin is severely scarred, even though others see no noticeable blemishes. |
| Mirror Checking | Frequently checking one’s appearance in mirrors or reflective surfaces. For example, someone may spend hours examining their face to check for perceived imperfections. |
| Avoidance of Social Situations | Avoiding social interactions due to fear of being judged based on appearance. For example, someone may avoid gatherings because they believe others will criticize their facial features. |
| Excessive Grooming | Engaging in excessive grooming to fix or hide perceived defects. For example, someone may spend hours styling their hair or applying makeup to cover their perceived flaws. |
| Comparing to Others | Constantly comparing one’s appearance to others. For example, someone may feel inferior when comparing their body shape to others at the gym. |
| Cosmetic Procedures | Seeking unnecessary cosmetic surgeries or treatments. For example, someone may undergo multiple cosmetic surgeries to alter a facial feature they are unhappy with, despite reassurances from professionals that no procedure is needed. |
Causes and Risk Factors of Body Dysmorphic Disorder (BDD)
The exact causes of BDD are not fully understood, but it is believed to result from a combination of genetic, biological, and environmental factors. Certain risk factors may increase the likelihood of developing BDD or its subtype, Muscle Dysmorphia.
1. Genetic and Biological Factors
Research suggests that BDD may have a genetic component, as individuals with a family history of anxiety, depression, or obsessive-compulsive disorder (OCD) may be more likely to develop the condition. Neurotransmitter imbalances, particularly in serotonin, are also thought to contribute to the disorder.
- Twin and family studies have shown that genetic factors play a role in the development of BDD. Individuals with first-degree relatives who have BDD or related disorders may be at higher risk.
- Neuroimaging studies suggest that abnormalities in brain regions involved in visual processing and emotional regulation may contribute to the distorted body image seen in BDD.
2. Environmental and Psychological Factors
Environmental stressors, such as bullying, teasing, or societal pressure to conform to specific beauty standards, can trigger the development of BDD. Individuals who have experienced body shaming or pressure to achieve a certain appearance may be more vulnerable to developing the disorder.
- Cultural factors, such as the emphasis on physical appearance in media and social media, may contribute to the onset of BDD. Exposure to unrealistic beauty ideals can increase body dissatisfaction and trigger obsessive concerns about appearance.
- Psychological factors, including low self-esteem, perfectionism, and a history of anxiety or depression, are also associated with BDD.
Therapy and Treatment Options for Body Dysmorphic Disorder (BDD)
Treating BDD involves a combination of therapeutic interventions that target both the obsessive thoughts and compulsive behaviors associated with the disorder. Below are key treatment options:
1. Cognitive Behavioral Therapy (CBT)
CBT is the most effective therapy for treating BDD, particularly through a specific form called Exposure and Response Prevention (ERP). CBT helps individuals challenge their negative beliefs about their appearance and resist engaging in compulsive behaviors such as mirror checking or excessive grooming.
Example: Samantha, who struggles with obsessive thoughts about her nose, works with her CBT therapist to gradually reduce her mirror-checking behaviors. Through ERP, she learns to tolerate the anxiety associated with not checking her appearance and begins to challenge her distorted beliefs about her nose.
2. Mindfulness-Based Cognitive Therapy (MBCT)
MBCT combines mindfulness practices with cognitive therapy to help individuals become more aware of their thoughts and feelings without becoming overwhelmed by them. This therapy is particularly useful for managing the obsessive thoughts that drive compulsive behaviors in BDD.
Example: Jake, who has Muscle Dysmorphia, learns through MBCT how to observe his negative thoughts about his body without reacting to them. By practicing mindfulness, he is able to reduce his compulsive exercise routines and focus on healthier, more balanced fitness goals.
3. Pharmacotherapy (Medication Management)
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to help manage the symptoms of BDD. These medications help regulate serotonin levels in the brain, reducing both obsessive thoughts and compulsive behaviors.
Example: Jake’s psychiatrist prescribes an SSRI to help regulate his mood and reduce the intensity of his preoccupation with muscle size. With medication and therapy, Jake experiences
Long-Term Management of Body Dysmorphic Disorder (BDD)
Managing BDD over the long term requires consistent therapeutic intervention and a commitment to treatment. Below are key strategies for long-term management:
- Regular Therapy: Continued participation in therapies such as CBT and MBCT helps individuals develop effective coping strategies to manage obsessive thoughts and compulsive behaviors.
- Medication Adherence: For individuals taking SSRIs or other medications to manage their symptoms, consistent use of medication is essential for maintaining stability.
- Support Networks: Engaging with supportive family, friends, or support groups provides emotional support and helps individuals stay motivated in their treatment.
- Body Positivity and Self-Acceptance: Encouraging self-acceptance and body positivity through therapy and self-care practices can help individuals with BDD develop healthier attitudes toward their appearance.
Conclusion
Body Dysmorphic Disorder (BDD) is a serious mental health condition that can significantly impair an individual’s quality of life, particularly when complicated by subtypes such as Muscle Dysmorphia. However, with the right combination of treatments—such as Cognitive Behavioral Therapy, Mindfulness-Based Cognitive Therapy, and pharmacotherapy—individuals can manage their symptoms and lead fulfilling lives. Long-term management strategies, including regular therapy, medication adherence, and support networks, are essential for maintaining stability and preventing relapse.
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Link
- Nolen-Hoeksema, S. (2014). Abnormal Psychology. McGraw-Hill Education.
- Phillips, K. A. (2009). Understanding Body Dysmorphic Disorder: An Essential Guide. Oxford University Press.
- Craske, M. G., & Barlow, D. H. (2007). Mastery of Your Anxiety and Depression: Workbook (Treatments That Work). Oxford University Press.
- Veale, D., & Neziroglu, F. (2010). Body Dysmorphic Disorder: A Treatment Manual. Wiley-Blackwell.
Explore Other Mental Health Issues