Contents
Introduction
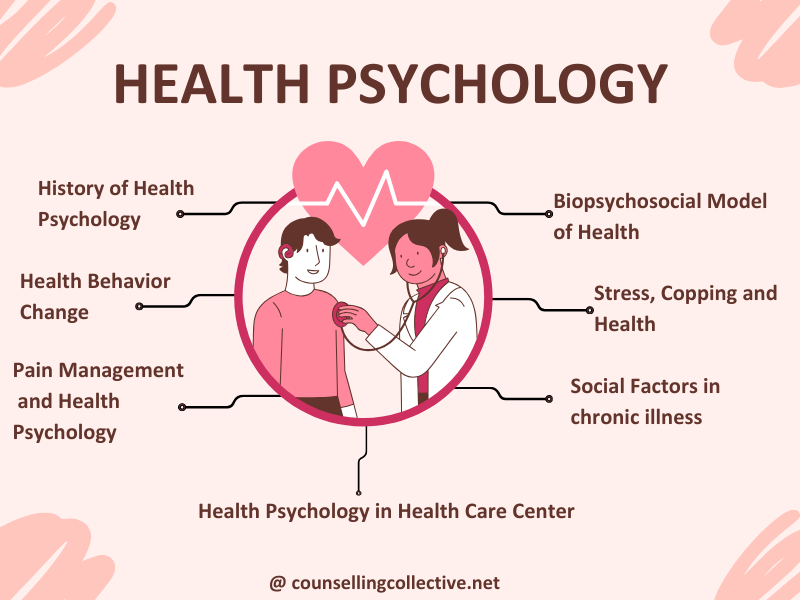
Health psychology is a dynamic field that examines the interplay between psychological processes and overall health and well-being.
It focuses on understanding health behaviors, it describes psychological intricacies governing choices vital to overall well-being. In chronic illness, Health Psychology rigorously examines the impact of social factors on health outcomes, guided by the encompassing Biopsychosocial Model.
In this article, we will explore the impact of social factors on health outcomes in chronic illness, guided by the encompassing Biopsychosocial Model.
Mind and Body Connection in Health Psychology
Health Psychology emphasizes the importance of incorporating psychological interventions alongside medical treatments. It recognizes that mental well-being is closely intertwined with physical health. Such as;
- Stress Management: Techniques such as mindfulness and cognitive-behavioral therapy can reduce stress and improve immune function.
- Behavioral Interventions: Strategies like exercise and healthy eating are promoted to enhance both mental and physical health.
- Support Systems: Building strong social support networks can improve recovery rates and overall health outcomes.
- Pain Management: Psychological approaches, including relaxation techniques and biofeedback, can help manage chronic pain.
- Adherence to Treatment: Counseling and motivational interviewing can enhance patients’ adherence to medical regimens.
History of Health Psychology
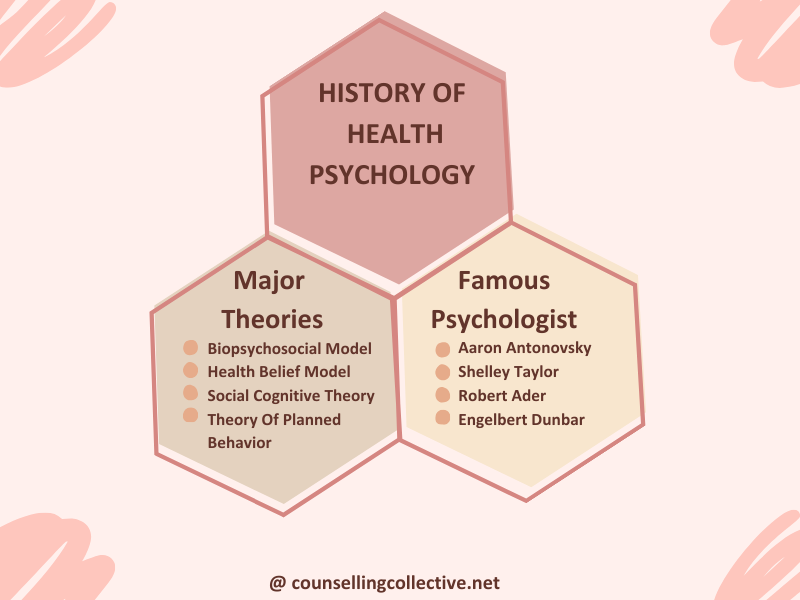
The history of health psychology is a fascinating journey that has evolved over the last few decades. Health psychology is a subfield of psychology that focuses on how psychological, social, and behavioral factors influence health and illness.
In this section, we will explore
- Psychologists who shaped the field of health psychology
- Major Theories of Health Psychology
Major Theories of Health Psychology
Health Psychology has evolved over the years, drawing from various theories and perspectives to understand the complex relationship between psychology and health. Some of the major theories that have shaped the field include;
- Biopsychosocial Model: Proposes that health and illness result from a combination of biological, psychological, and social factors. Key components include biological processes, psychological factors (thoughts, emotions, behaviors), and social influences.
- Health-Belief Model: Suggests that individuals’ health-related behaviors are influenced by their beliefs and perceptions. Key factors include perceived susceptibility, severity, benefits, barriers, and cues to action.
- Social Cognitive Theory: Emphasizes observational learning and self-efficacy in health-related behaviors. Key components include observational learning, self-efficacy, role models, social context, and self-regulation.
- Theory of Planned Behavior: Focuses on an individual’s intention to engage in a behavior, influenced by attitudes, subjective norms, and perceived behavioral control. Key components include attitudes toward behavior, subjective norms, perceived behavioral control, and behavioral intentions.
Psychologists Who Shaped The Field Of Health Psychology
Several influential psychologists have significantly contributed to the development and establishment of Health Psychology as a distinct field. Their work has paved the way for understanding the psychological factors that impact health outcomes. Some notable psychologists who have shaped the field of Health Psychology include:
- George Engel: Developed the Biopsychosocial Model, revolutionizing the understanding of health and illness by integrating biological, psychological, and social factors. This model highlights the complex interplay between different dimensions of health.
- Albert Bandura: Known for Social Cognitive Theory, which emphasizes the impact of observational learning and self-efficacy on health-related behaviors. His work has significantly influenced how individuals approach and manage their health.
- Irwin Rosenstock: Created the Health-Belief Model, outlining how personal beliefs and perceptions influence health behaviors and decision-making. His model has contributed to the development of preventive health strategies and interventions.
- Icek Ajzen: Developed the Theory of Planned Behavior, exploring how attitudes, subjective norms, and perceived behavioral control affect health-related intentions and actions. This theory provides a framework for understanding and predicting health behaviors.
Health Psychology and Chronic Illness.
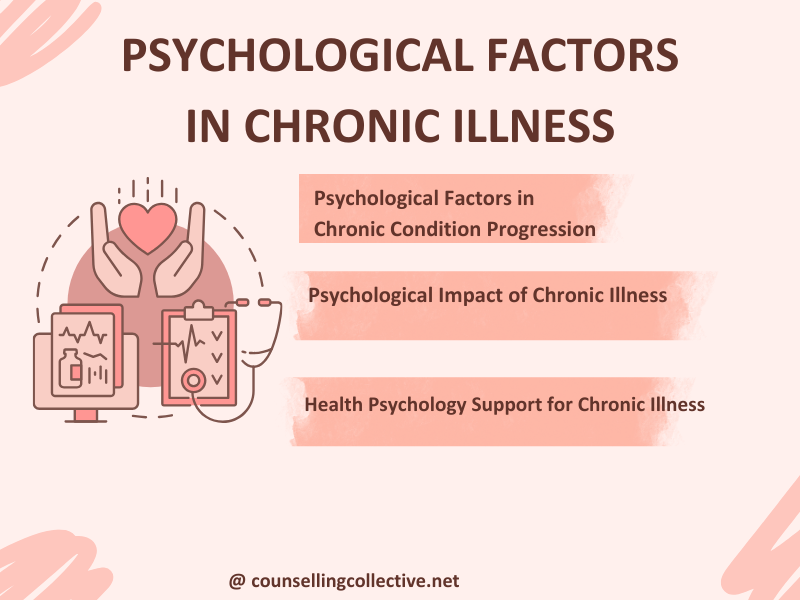
Chronic illness involves conditions that persist over an extended period and often require ongoing medical attention. Psychological factors play a significant role in how individuals experience, cope with, and manage chronic illnesses.
In this section, we will explore
- Health psychology
- Psychological Impact of Chronic Illnes
- Psychological Factors in Chronic Condition Progression
Health psychology plays a crucial role in pain management by addressing the psychological factors that influence pain perception and implementing interventions to improve overall pain management. By integrating psychological approaches with medical treatments, health psychology offers a holistic perspective on managing pain.
Psychological Impact of Chronic Illness
Living with a chronic illness can have profound psychological implications for individuals. The experience of managing a long-term health condition can lead to a range of emotional and psychological challenges. Some common psychological implications include
| Psychological Factor | Impact on Chronic Condition Progression |
| Emotional Distress | Can exacerbate symptoms and accelerate disease progression due to chronic stress. Emotional distress may lead to poor self-care and adherence to treatment. |
| Stress and Coping Mechanisms | Effective coping strategies can help manage symptoms and improve quality of life. Poor stress management can lead to worsened health outcomes and increased symptom severity |
| Self-Esteem and Identity | Changes in self-esteem and identity due to chronic illness may affect adherence to treatment and engagement in self-care activities. Low self-esteem can negatively impact health behaviours. |
| Social Isolation | Reduced social support and increased isolation can lead to worsened psychological well-being and hinder effective management of the condition. Social isolation can negatively affect health outcomes. |
| Adjustment to Lifestyle Changes | Difficulty in adapting to necessary lifestyle changes can impact disease management and overall health. Effective adjustment is crucial for maintaining treatment adherence and managing symptoms. |
Psychological Factors in Chronic Condition Progression
- Emotional Distress: Chronic illness often leads to feelings of anxiety, depression, and frustration due to the persistent nature of the condition and its impact on daily life.
- Adjustment Issues: Patients may struggle with adapting to lifestyle changes and limitations imposed by their illness, leading to a sense of loss and decreased quality of life.
- Social Isolation: The need for frequent medical appointments and physical limitations can result in reduced social interactions and feelings of loneliness.
- Self-Identity: Chronic illness can alter a person’s self-perception and identity, as they may see themselves primarily as a patient rather than an individual.
- Coping Mechanisms: Developing effective coping strategies is crucial. Some patients may benefit from psychological interventions such as cognitive-behavioral therapy to manage stress and emotional responses.
Pain Management and Health Psychology
Pain management in health psychology focuses on understanding and alleviating chronic pain through psychological interventions. Techniques such as cognitive-behavioral therapy, are employed to reduce pain perception, improve daily functioning, and enhance overall quality of life for patients.
In this section, we will explore
- Psychological Influences on Pain Perception
- Health Psychology Interventions for Effective Pain Management

Psychological Influences on Pain Perception
- Emotional States: Emotions such as anxiety, depression, and stress significantly impact how pain is perceived. High levels of emotional distress can amplify pain sensitivity and contribute to a heightened pain experience. Conversely, positive emotions and effective emotional regulation can help reduce pain perception and improve coping.
- Cognitive Processes: How individuals interpret and think about their pain can influence their pain experience. Cognitive factors such as catastrophic thinking (e.g., fearing that pain will worsen) can exacerbate the sensation of pain. Cognitive distortions and negative thought patterns can lead to increased pain and emotional distress, making effective cognitive management a key component of pain management.
- Attention and Focus: The ability to focus attention away from pain can influence pain perception. Techniques that help individuals divert their attention from pain, such as engaging in activities or practicing mindfulness, can reduce the intensity of pain experienced. Distraction strategies and techniques to refocus attention play a vital role in managing chronic pain.
- Behavioral Responses: Pain-related behaviors, such as avoidance or inactivity, can affect pain intensity and progression. For example, avoiding physical activity due to pain can lead to increased deconditioning and exacerbation of symptoms. Behavioral responses to pain, including how individuals manage and respond to their pain, impact overall pain management.
Health Psychology Interventions for Effective Pain Management
| Intervention | Description | Benefits |
| Cognitive-Behavioral | Focuses on changing negative thought patterns and behaviours related to pain. Utilises techniques such as cognitive restructuring and behavioural strategies. | Reduces emotional distress, improves coping skills, and enhances overall functioning. |
| Mindfulness-Based Stress Reduction | Involves mindfulness meditation and body awareness practices to promote acceptance and reduce the emotional impact of pain. | Enhances pain management, reduces stress, and improves overall well-being. |
| Biofeedback | Teaches individuals to control physiological processes like muscle tension and heart rate through real-time feedback. | Increases awareness and self-regulation, helping to manage pain more effectively. |
| Relaxation Techniques | Includes methods such as progressive muscle relaxation, deep breathing exercises, and guided imagery to reduce physical tension and stress. | Lowers pain perception, improves comfort, and promotes relaxation. |
| Behavioural Activation | Encourages engagement in meaningful activities despite the presence of pain. Focuses on counteracting pain-related inactivity. | Enhances mood, quality of life, and reduces the impact of pain on daily activities. |
| Supportive Counselling | Provides emotional support and helps individuals address the psychological challenges associated with chronic pain. | Offers a safe space to discuss pain-related issues, helping manage the emotional impact. |
Ethical Considerations in Integrating Health Psychology Into Healthcare
Integrating Health Psychology into healthcare settings requires careful consideration of ethical principles to ensure the well-being and rights of both patients and practitioners. Here are some key ethical considerations in this integration:
- Informed Consent: Health psychologists must secure informed consent before beginning any interventions or assessments, ensuring patients understand the purpose, procedures, risks, benefits, and alternatives. This respects patient autonomy and ensures voluntary participation.
- Confidentiality and Privacy: Health psychologists must protect patient confidentiality and privacy, including secure data handling and obtaining written consent before sharing information. They must also clearly communicate any limits to confidentiality, especially when safety is at risk.
- Competence: Health psychologists should practice within their areas of expertise and stay updated with current research. Continuous professional development is essential to avoid ineffective or harmful interventions.
- Dual Relationships: Avoiding dual relationships is crucial to prevent conflicts of interest and maintain professional boundaries. This helps ensure that the therapeutic relationship remains focused solely on the patient’s well-being.
- Cultural Sensitivity: Health psychologists need to be culturally sensitive, understanding how cultural factors influence health beliefs and practices. Tailoring interventions to respect diverse perspectives ensures more effective and respectful care.
Focus Areas in Health Psychology Research and Practice
In Health Psychology, research and practice cover a wide range of key areas that contribute to understanding and promoting overall well-being. Some of the prominent areas of focus include these.
- Health Behavior Change: Health psychology uses techniques like motivational interviewing and behavior modification to encourage healthier lifestyles, improving diet, exercise, and overall well-being.
- Stress and Coping: Research focuses on managing stress through relaxation techniques, cognitive-behavioral therapy, and resilience training, aiming to reduce stress and enhance mental health.
- Patient-Provider Communication: Effective communication fosters accurate diagnosis, treatment adherence, and patient satisfaction, emphasizing empathy and open dialogue for better health outcomes.
- Psychosocial Factors in Health: Social support, socioeconomic status, and cultural beliefs significantly influence health outcomes, essential for comprehensive health assessments.
- Chronic Illness Management: Health psychology improves coping strategies and treatment adherence, enhancing the quality of life for chronic illness patients.
- Pain Management: Cognitive-behavioral therapy, relaxation techniques, and biofeedback reduce pain perception and improve daily functioning.
- Health Promotion and Disease Prevention: Public health campaigns, health education, and targeted interventions encourage preventive behaviors, reducing health risks and enhancing population health.
Conclusion
Health psychology sheds light on the deep connections between our minds and bodies, especially when dealing with chronic illness. By blending psychological support with medical care, it helps people manage their health more effectively and live better lives. The insights from key theories and pioneering psychologists in this field guide us toward more compassionate and holistic healthcare. Through this approach, health psychology continues to make a meaningful difference in people’s lives.
References
- Baum, A., & Stanford, G. (2001). Health psychology: A biopsychosocial approach (2nd ed.). Amazon
- Feuerstein, M., Labbé, E. E., & Kuczmierczyk, A. R. (1986). Health Psychology: A Psychobiological Perspective (1986th ed.). Amazon.
- Miller, W. R., & Rollnick, S. (2012). Motivational Interviewing: Helping People Change. Amazon
- Rabin, B. S., Ph.D., M.D. (2019). Coping with Stress for Mental and Physical Health and Longevity. Amazon
- Brownridge, K. L.. 50 Things to Know About Coping With Stress: By A Mental Health Specialist (50 Things to Know Coping With Stress) [Kindle Edition].Amazon
- Maté, G., M.D. (2011). When the Body Says No: Exploring the Stress-Disease Connection. Amazon
- Caudill, M. A., & Benson, H.Managing Pain Before It Manages You (Fourth Edition) [Paperback]. Amazon
- Zoffness, R., MS PhD, & Schumacher, M. A., MD PhD. (2020). The Pain Management Workbook: Powerful CBT and Mindfulness Skills to Take Control of Pain and Reclaim Your Life [Paperback]. Amazon
- Bor, R., Miller, R., & Gill, S. Counseling in Health Care Settings: A Handbook for Practitioners (Professional Handbooks in Counselling and Psychotherapy),( 6th Edition). Amazon