Contents
Introduction

Cognitive Behavioral Therapy: Theory, Therapy & Applications
Cognitive Behavioral Therapy (CBT) is a widely recognized therapeutic approach that focuses on transforming negative thoughts and behaviors. It’s proven effective for treating a range of mental health issues by offering practical, actionable strategies for change. In this article, we will understand CBT Theory with different perspectives, see its applications as therapy, debunk common myths about CBT and look into its limitations.
Without further wait, lets dive into the world of CBT.
What is Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy (CBT) is a type of psychotherapy that focuses on changing unhelpful or destructive thought patterns, which in turn can alter behaviors and emotions. Developed in the 1960s by psychiatrist Aaron Beck, CBT is grounded in the belief that our thoughts, feelings, and behaviors are interconnected, and that by changing one, we can influence the others.
CBT has gained widespread popularity due to its evidence-based approach and effectiveness in treating a variety of mental health conditions, such as anxiety, depression, and post-traumatic stress disorder (PTSD) (Beck Institute for Cognitive Behavior Therapy).
Why CBT is Important
CBT is particularly important because it empowers individuals to take control of their mental health by learning practical skills that they can apply in their daily lives. Unlike other forms of therapy that might delve into the past to uncover underlying causes of distress, CBT is future-oriented and focused on problem-solving in the present.
CBT’s effectiveness has been extensively studied, and it is often compared to other therapeutic approaches. For example, while psychoanalysis might require years of therapy to see significant changes, CBT typically shows results in a shorter period—often within 12-20 sessions (American Psychological Association).
Different Types of CBT
- Dialectical Behavior Therapy (DBT): Originally developed to treat borderline personality disorder, DBT combines principles of Cognitive Behavioral Therapy (CBT) with mindfulness and acceptance strategies. It focuses on teaching skills for emotion regulation, distress tolerance, and improving interpersonal effectiveness. DBT helps clients manage intense emotions, reduce self-destructive behaviors, and navigate conflicts more effectively.
- Acceptance and Commitment Therapy (ACT): ACT emphasizes accepting thoughts and feelings without trying to change or avoid them, while committing to behaviors that align with one’s core values. which is particularly useful in managing conditions like chronic pain, anxiety, depression, and stress. ACT combines mindfulness techniques with behavioral change strategies to help clients live a more meaningful and fulfilling life, even in the presence of difficult emotions.
- Mindfulness-Based Cognitive Therapy (MBCT): MBCT integrates mindfulness practices with Cognitive Behavioral Therapy (CBT) principles to prevent the recurrence of depression, especially in individuals with a history of multiple episodes. It focuses on helping individuals become more aware of their thoughts, emotions, and bodily sensations without becoming overwhelmed by them.
Understanding How CBT Works
Cognitive Behavioral Therapy (CBT) operates on the principle that our thoughts, emotions, and behaviors are interconnected. Negative thought patterns can lead to negative emotional responses and behaviors, creating a self-perpetuating cycle. CBT aims to break this cycle by challenging and altering these negative thought patterns.
Now we will see CBT from three different level of details. First the simple overview then and then summarized in-depth analysis.
Simple Overview
Core Idea CBT is based on the understanding that our thoughts influence our emotions and behaviors. Negative thoughts can lead to negative feelings and actions, reinforcing the negative cycle. CBT helps break this cycle by identifying and changing these negative thoughts.
Real-Life Example Imagine you’re preparing for a big presentation and think, “I’m going to mess this up.” This thought might make you feel anxious and lead to avoiding preparation or performing poorly. CBT would help you:
- Replace with a Balanced Thought: Transform the negative thought into a more balanced and realistic one, such as, “I have prepared well and will do my best.” This reframing helps to reduce anxiety and improve performance by focusing on effort and preparation rather than potential failure.
- Challenge the Thought: Evaluate the accuracy and validity of the negative thought by examining the evidence for and against it. Ask yourself, “Is there concrete proof that I will mess this up?” or “Have I succeeded in similar situations before?” By challenging the thought, you can uncover irrational or exaggerated beliefs and replace them with more realistic and constructive thinking.
Detailed Concepts
CBT includes core components such as cognitive restructuring, behavioral activation, and exposure therapy.
- Cognitive Restructuring: Cognitive Restructuring is a therapeutic technique used to identify and challenge irrational or maladaptive thoughts that contribute to negative emotions and behaviors. For instance, a student might catastrophize a potential failure on a test with thoughts like, “If I fail, my life is over.”
- Behavioral Activation: Behavioral Activation is a technique primarily used to treat depression by encouraging clients to engage in activities that promote positive reinforcement and enhance mood. Depression often leads to avoidance and withdrawal from activities that once brought pleasure or a sense of accomplishment.
- Exposure Therapy: Exposure Therapy is a widely used technique in the treatment of anxiety disorders, such as phobias, panic disorder, and social anxiety. This approach involves gradually exposing individuals to feared situations, objects, or thoughts in a controlled and safe environment. The goal is to reduce avoidance behaviors and help individuals confront their fears directly.
In-Depth Analysis
CBT’s theoretical underpinnings are deeply rooted in the cognitive model, which posits that our thoughts (cognitions) influence our emotions and behaviors. This model is often associated with Beck’s work on depression, where he identified negative cognitive distortions like all-or-nothing thinking, overgeneralization, and catastrophizing.
- Schema Theory: Schema Theory is a key concept in Cognitive Behavioral Therapy (CBT) that highlights the role of deeply ingrained beliefs, or “schemas,” in shaping how individuals perceive, interpret, and respond to their experiences. Schemas are cognitive frameworks that develop early in life based on experiences and interactions and continue to influence thoughts and behaviors. For example, a person with a “failure schema” may perceive any mistake as evidence of their overall incompetence.
- Automatic Thoughts: Automatic thoughts are spontaneous, often subconscious thoughts that arise in response to specific situations and can significantly impact emotions and behaviors. In CBT, these thoughts are closely examined because they are typically quick, habitual, and often negative, leading to distressing emotional reactions.
Difference between CBT Theory and CBT Therapy
| Aspect | CBT Theory | CBT Therapy |
| Definition | TThe theoretical framework that explains the relationship between thoughts, feelings, and behaviors. | The application of CBT principles through practical techniques to address specific psychological issues. |
| Core Concepts | – Cognitive Distortions: Systematic errors in thinking. – Cognitive Model: How thoughts influence emotions and behaviors. – Negative Automatic Thoughts: Spontaneous, negative thoughts that influence mood and behavior. | – Cognitive Restructuring: Identifying and challenging negative thought patterns. – Behavioral Experiments: Testing beliefs through real-life experiments. – Exposure Therapy: Gradual exposure to feared situations to reduce avoidance. – Skills Training: Teaching coping strategies and problem-solving skills. |
| Purpose | To explain how psychological problems develop and persist and how altering thought patterns can improve outcomes | To help individuals address psychological issues by applying techniques to change thoughts and behaviors |
| Development | Developed from cognitive psychology (e.g., Aaron Beck) and behavioral psychology (e.g., B.F. Skinner), integrating theories about cognition and behavior. | Developed as a practical method for therapists to implement the principles of CBT Theory, focusing on symptom relief and behavioral change. |
| Application | Provides the rationale for why certain therapeutic techniques are effective based on theoretical understanding. | Delivered through structured sessions by therapists, often with homework and exercises |
Notable Psychologists in CBT
Cognitive Behavioral Therapy (CBT) has been significantly shaped by the work of several pioneering psychologists. These individuals have contributed to its development, refinement, and application across various psychological conditions. Here are some key figures:

- Aaron T. Beck: Often called the “father of cognitive therapy,” Beck developed CBT in the 1960s, focusing on how negative thoughts influence emotions and behaviors. His work on cognitive restructuring and the cognitive model laid the foundation for modern CBT (Beck Institute).
- Albert Ellis: Ellis created Rational Emotive Behavior Therapy (REBT), a precursor to CBT. He emphasized the role of irrational beliefs in emotional distress and introduced the ABC model, which is still a core component of CBT (Albert Ellis Institute).
- David D. Burns: A student of Aaron Beck, Burns popularized CBT through his book “Feeling Good: The New Mood Therapy.” He introduced the concept of cognitive distortions and practical techniques for challenging them, making CBT accessible to the public (David D. Burns, M.D.).
- Judith S. Beck: Judith Beck, the daughter of Aaron Beck, has advanced CBT, particularly in the areas of weight loss and eating disorders. As president of the Beck Institute, she has authored numerous influential books and training programs (Beck Institute).
- Donald Meichenbaum:: Meichenbaum developed Cognitive Behavioral Modification (CBM) and introduced Stress Inoculation Training (SIT), broadening the application of CBT to a range of psychological and behavioral issues (Donald Meichenbaum).
CBT Theory & Therapy in Treating Mental Health Disorders
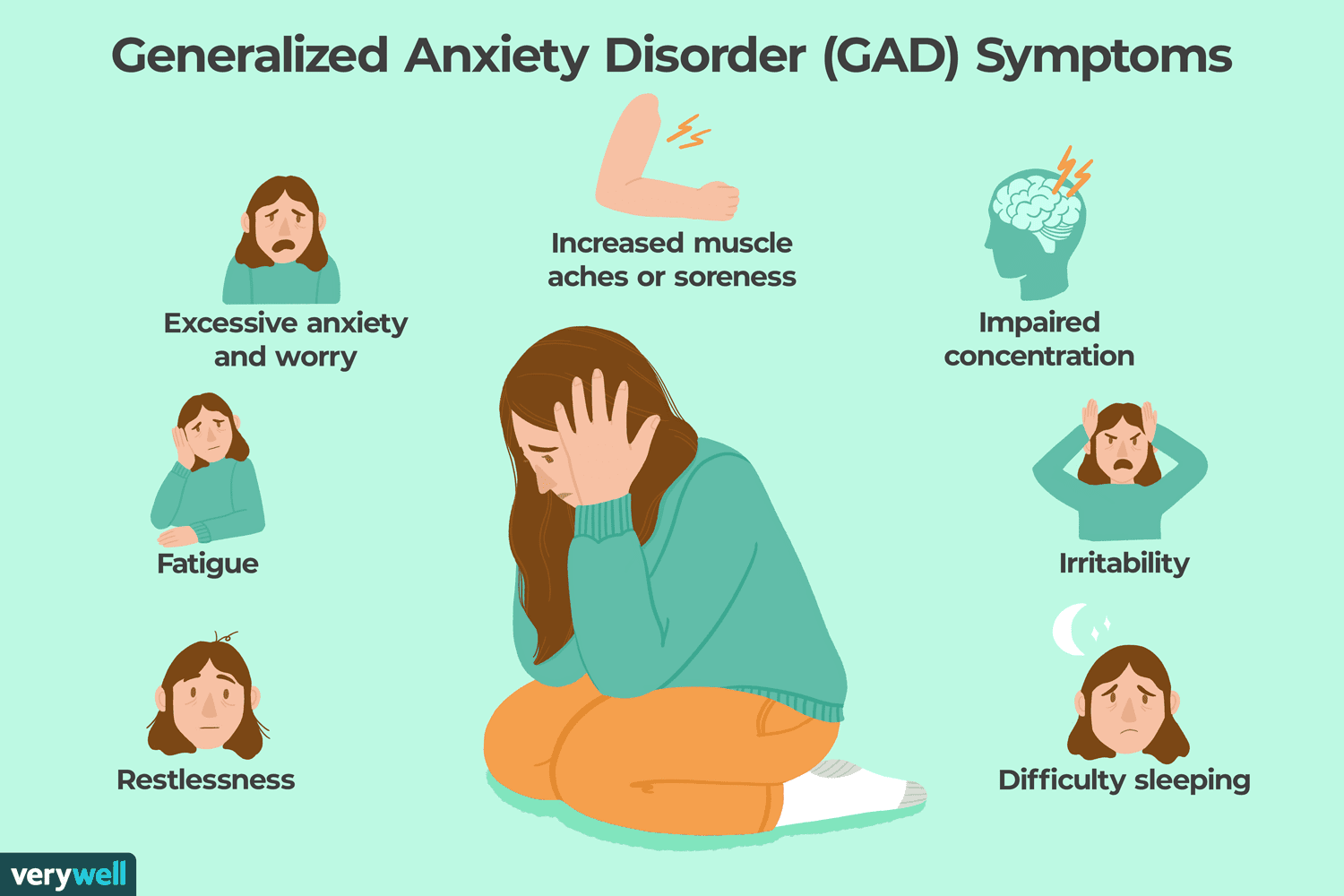
CBT is one of the most effective treatments for anxiety disorders. Specific techniques like exposure therapy are particularly useful in treating phobias, panic disorder, and generalized anxiety disorder (GAD).
Example: Consider Jane, who suffers from a severe phobia of flying. Her therapist uses gradual exposure therapy, starting with watching videos of planes, then visiting an airport, and eventually taking a short flight. Alongside exposure, Jane works on cognitive restructuring to challenge her belief that “flying is dangerous” by focusing on facts and statistics that demonstrate its safety.
Image Source: Verywell / Cindy Chung
CBT addresses depression by helping clients recognize and change negative thought patterns that contribute to their low mood. Techniques like behavioral activation, where clients are encouraged to engage in enjoyable activities even when they don’t feel like it, can help break the cycle of inactivity and despair.
Example: Tom feels hopeless and spends most days in bed, believing that “nothing will ever get better.” His therapist works with him to identify small, achievable goals, like taking a short walk each day. Over time, these activities help lift his mood, and he begins to challenge his negative beliefs with evidence of positive changes in his life.
Image Source: republicpolicy.com

Post-Traumatic Stress Disorder
CBT, particularly in the form of trauma-focused CBT, is highly effective in treating PTSD. Cognitive restructuring helps clients process and reframe traumatic memories, while exposure therapy can help reduce the distress associated with these memories.
Example: Sarah, a survivor of a car accident, avoids driving and experiences flashbacks whenever she sees a car. Her therapist uses a combination of cognitive restructuring to challenge her belief that “driving is always dangerous” and gradual exposure therapy, where she starts by sitting in a parked car and slowly progresses to driving short distances.
Image Source: teachermagazine.com

Obsessive-Compulsive Disorder
For OCD, CBT often involves exposure and response prevention (ERP), where clients are exposed to situations that trigger their obsessions but are encouraged not to engage in their usual compulsive behaviors (International OCD Foundation).
Example: John has a compulsion to wash his hands repeatedly, fearing contamination. In ERP, his therapist encourages him to touch a doorknob (a feared object) and then refrain from washing his hands, gradually reducing the anxiety associated with not performing the compulsion.
Image Source: psychicare.com
Common Myths About CBT
| Myth | Fact |
| CBT is only for severe mental disorders | CBT is versatile and can help with a wide range of issues, including stress, anxiety, depression, and everyday problems. It is designed to be accessible and practical for various levels of mental health concerns. |
| CBT is just positive thinking | While CBT does involve modifying negative thought patterns, it goes beyond positive thinking. It includes identifying cognitive distortions, understanding their impact, and developing strategies to change these patterns through evidence-based techniques. |
| CBT is a quick fix | Although CBT can lead to noticeable improvements relatively quickly, it is not a “quick fix.” It requires a commitment to practice new skills, engage in behavioral experiments, and work through challenges to achieve and maintain long-term change. |
| CBT ignores emotions | CBT does not ignore emotions; instead, it helps individuals understand and manage them more effectively. By exploring how thoughts influence emotions and behaviors, CBT helps individuals develop healthier emotional responses and coping mechanisms |
| CBT is only for adults | CBT is adaptable for all age groups, including children and adolescents. Techniques and language are adjusted to be age-appropriate, and CBT can be particularly effective for young people dealing with anxiety, depression, and other issues. |
Criticisms and Limitations
- Oversimplification: CBT is criticized for potentially oversimplifying complex mental health issues by focusing mainly on thoughts and behaviors while neglecting deeper emotional processing. Critics argue that it may not fully address underlying causes, such as childhood trauma or personality disorders.
- Effectiveness for Deep-Seated Issues: CBT may be less effective for individuals with deep-seated personality disorders or those who struggle with the structured, problem-solving approach required by CBT. The emphasis on homework and self-monitoring can also be overwhelming for some clients.
- Defense of CBT: Proponents argue that while CBT may not cover every aspect of psychological issues, it offers a practical and effective approach for managing symptoms and improving quality of life. CBT can also be integrated with other therapies, such as psychodynamic therapy or mindfulness-based approaches, to create a more comprehensive treatment plan.
Conclusion
Cognitive Behavioral Therapy (CBT) is a versatile and effective approach for addressing a variety of mental health issues by focusing on altering negative thought patterns and behaviors. Its structured methods, including cognitive restructuring, behavioral activation, and exposure therapy, have demonstrated significant success in treating conditions such as anxiety, depression, and PTSD. While CBT may have limitations, its practical, evidence-based techniques provide valuable tools for improving mental well-being and can be integrated with other therapies for a more comprehensive treatment approach.
References
- Beck, A. T., & Dozois, D. J. A. (2011). Cognitive therapy: Current status and future directions. Annual Review of Clinical Psychology, 7, 1-28.
- Beck Institute for Cognitive Behavior Therapy. (n.d.). About CBT.
- Burns, D. D. (1989). The feeling good handbook. William Morrow and Company.
- Ellis, A. (1962). Reason and emotion in psychotherapy. Lyle Stuart.
- Meichenbaum, D. (1977). Cognitive-behavior modification: An integrative approach. Springer.
- American Psychological Association. (2019). Clinical practice guideline for the treatment of depression across three age cohorts.
- Judith S. Beck. (2020). Cognitive behavior therapy: Basics and beyond (2nd ed.). Guilford Press.
- International OCD Foundation. (n.d.). Exposure and response prevention (ERP).
- National Institute for Health and Care Excellence. (2011). Generalised anxiety disorder and panic disorder in adults: Management.
- Hofmann, S. G., Asnaani, A., Vonk, I. J. J., Sawyer, A. T., & Fang, A. (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive Therapy and Research, 36(5), 427-440.
Explore more Theories & Therapies